Can we treat cancer through reduced sugar uptake?
New research reveals the mechanism behind a cancer-relevant inhibition of human sugar transporting protein. The hope is that this will guide future drug design targeting sugar uptake mechanisms. This will ultimately lead to progress in a number of important common conditions, such as diabetes and cancer.
Tumors and cancer cells are highly dependent on sugar uptake to maintain their rapid growth rate. It has been proposed that a regulation or reduction of cellular sugar uptake might have therapeutic benefits. While not being a panacea, a reduction in cancer growth rate could allow other treatments time to reach full effect, and potentially could allow a much improved efficacy of other chemotherapeutics.
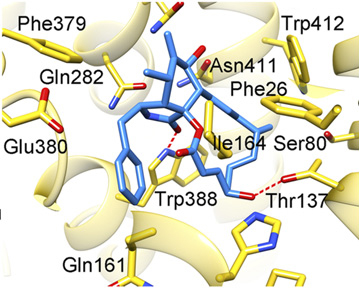
A research team from Aarhus University and the University of California San Francisco has revealed how different inhibitors of the human sugar transporter GLUT1 bind to a central cavity in the protein to inhibit its function. The results show a surprisingly promiscuous internal binding pocket with submicromolar affinities for chemically distinct substrates. With these results, the hope is that this will guide future drug design targeting sugar uptake mechanisms. This will ultimately lead to progress in a number of important common conditions, such as diabetes and cancer.
This is the first structures of GLUT1 in complex with inhibitors, and they provide a working template to develop cancer-therapeutic inhibitors. Cancer cells are dependent on greatly increased glucose consumption, and this dependence has been shown to result in up-regulation of glucose transporter expression, especially of GLUT1. The up-regulation of GLUT1 upon increased demand for glucose highlights it as an important prognostic indicator in several cancer types, as well as a potential new target for therapeutic inhibitors.
The new results show bound inhibitors that include the natural compound Cytochalasin B and two of a series of previously undescribed organic compounds binding in the submicromolar range. Cytochalasin B has been used extensively in the literature of GLUT1, and the results reveal its binding mode for the first time. However the most exciting result is that despite very different chemical backbones, all inhibitors tested bind in the same central cavity of the inward-open state of GLUT1, and all binding sites partly overlap the glucose-binding site. The results emphasize that modulation of glucose import by GLUTs should focus on making good interaction points for compounds, and that the actual chemical backbone of the inhibitor is of less importance.
“These insights are the result of several years of hard work from us,” says AIAS fellow and MBG Assistant Professor Bjørn Panyella Pedersen. “The experimental part of the project was mainly done at the University of California San Francisco (UCSF) and at Bayer Pharma AG in Germany, and fortunately we were able to collaborate and continue the project after my recruitment by AIAS to Aarhus University two years ago. It's a great joy to see the results on paper at last, and both my former mentor at UCSF, Prof. Robert Stroud, and myself will continue to push forward in this exciting and very competitive field.”
The results have just been published in Proceedings of the National Academy of Sciences (PNAS).
For further information, please contact
Assistant Professor Bjørn Panyella Pedersen
Aarhus Institute of Advanced Studies &
Department of Molecular Biology and Genetics
Aarhus University, Denmark
bpp@mbg.au.dk - Mobile: +45 2972 3499
